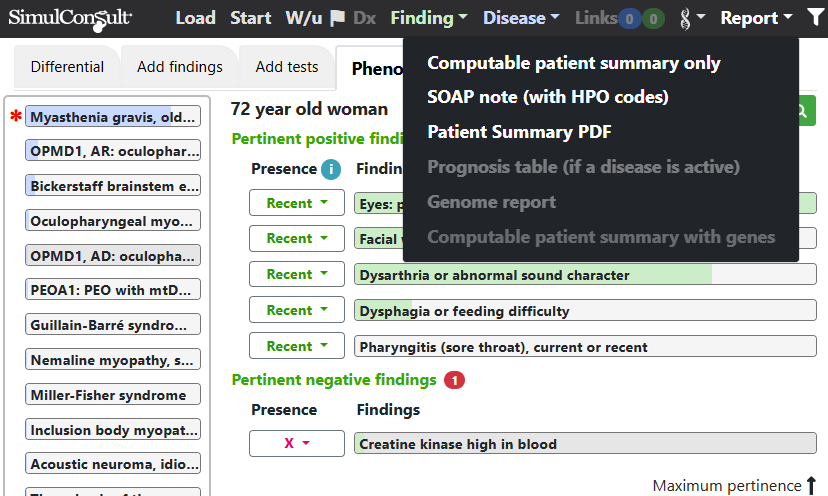
The SOAP (Subjective Objective Assessment Plan) note format has been changed to be in a more narrative style. It is accessible from Report on the top black navigation bar. The SOAP note display also contains a list of Human Phenotype Ontology (HPO) codes for findings present or absent in the patient. Some previous report outputs have been removed since their content is available in the new SOAP note.