Introduction
This is the first in an updated series of clinical cases to illustrate the power of SimulConsult in generating differential diagnoses in situations of substantial medical complexity. We will also demonstrate how SimulConsult continues to grow into a more powerful diagnostic tool via case-based quality improvement.
In this case, we are presented with a previously well woman with the sub-acute development of neurologic abnormalities among other seemingly unrelated clinical findings for which a unifying diagnosis required multiple hospitalizations and expert consultation to discover. It was not until after she had undergone multiple rounds of immunosuppressive therapies that a unifying genetic diagnosis was identified.
SimulConsult seeks to end diagnostic odysseys and errors, by empowering clinicians to reliably and quickly arrive at accurate differential diagnoses, order the right tests, and reach a confirmed diagnosis, and thus provide the best care for their patients.
Case Source
The below case was abstracted from the April 17th, 2024 edition of Case Records of the Massachusetts General Hospital from the New England Journal of Medicine. N Engl J Med 2024;390:1421-1430.
Patient Presentation
A 58-year-old woman presented with episodes of confusion and aphasia with brain MRI showing areas of T2-hyperintensity in the temporal lobe. Initial serological studies were negative for viral or bacterial etiologies. She was diagnosed with auto-immune encephalitis and underwent immunosuppressive therapies on multiple hospitalizations for recurrent episodes of symptoms. Below we provide a summary of clinical findings and test results that were abstracted from the clinical case and input in the SimulConsult software.
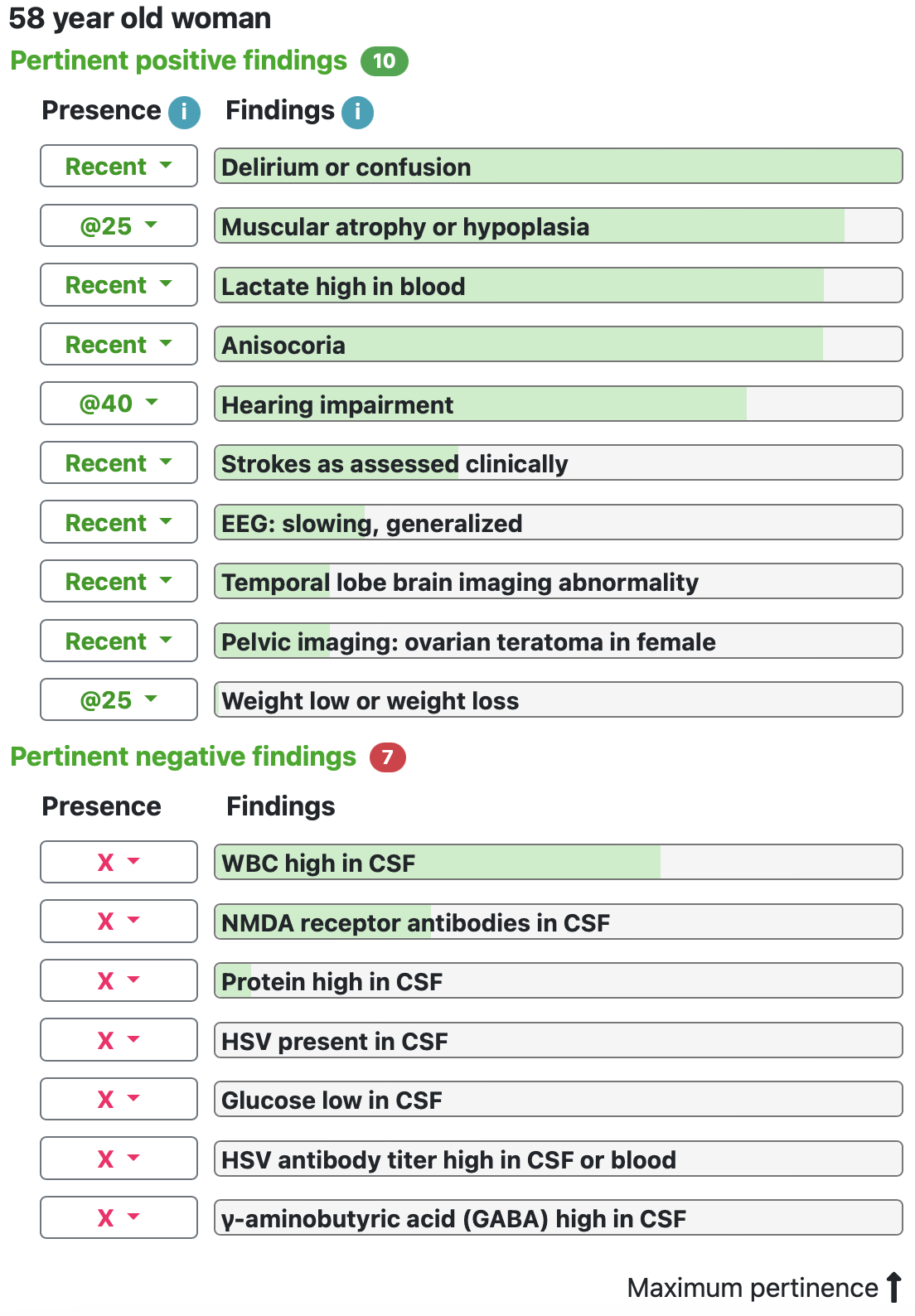
Initial SimulConsult Differential Diagnosis
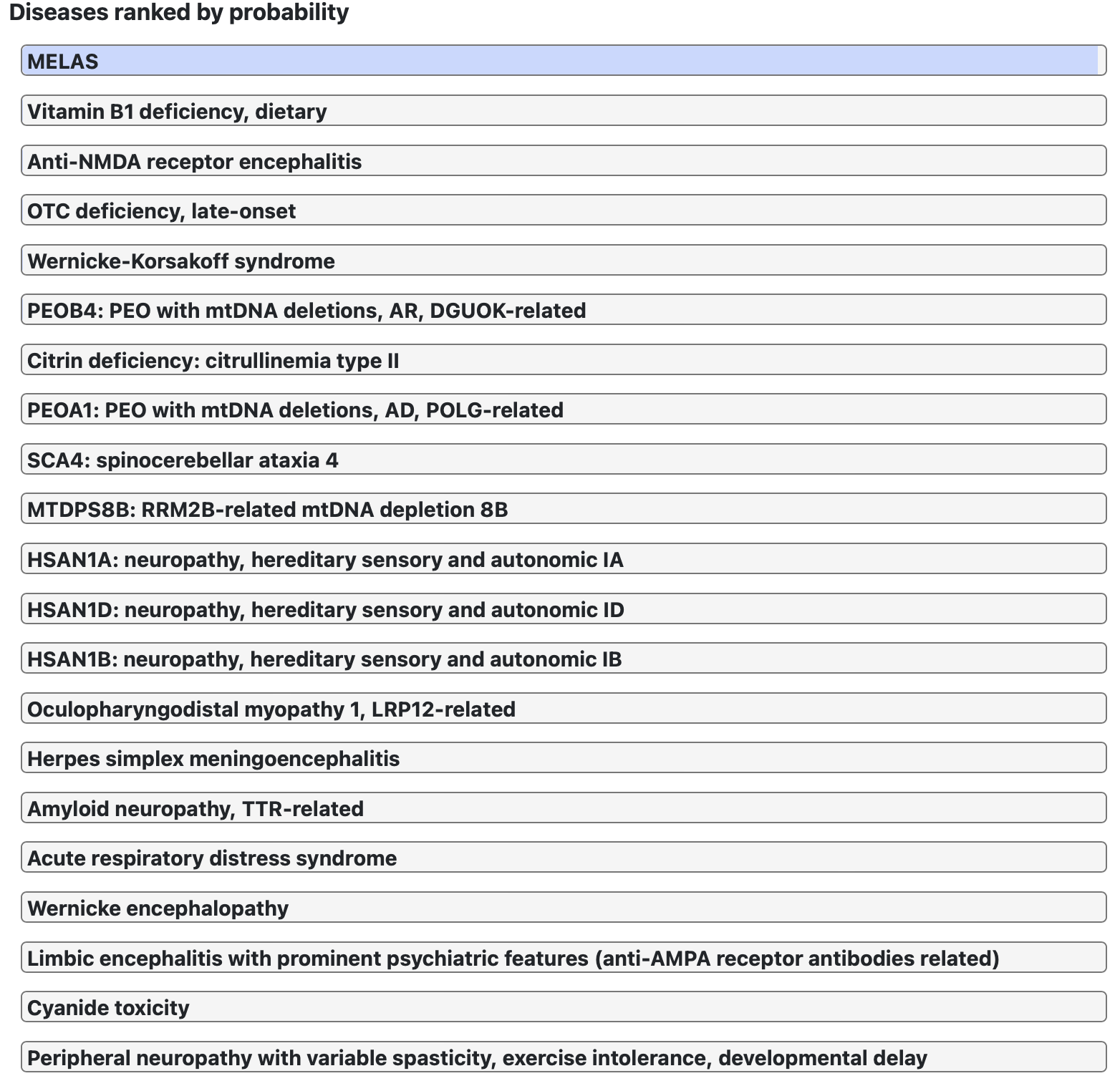
SimulConsult immediately identified the salient features of the patient’s presentation and provided a differential diagnosis including the following broad categories.
- Mitochondrial Disorder
- Autoimmune encephalitis
- Vitamin Deficiency
- Hereditary Neurological Disorders
- Infectious encephalitis
Visual explanation of each of top 3 diseases on differential
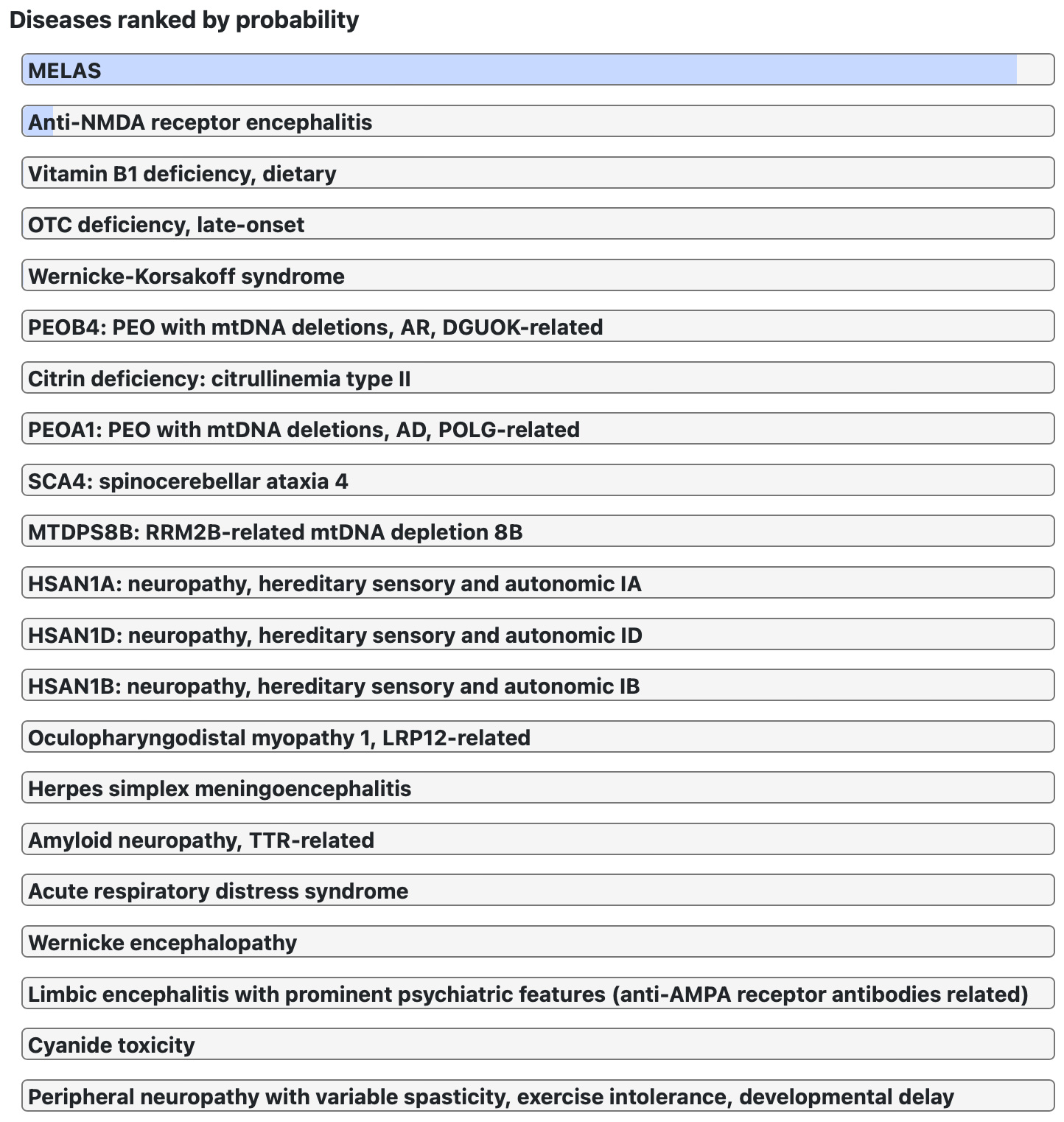
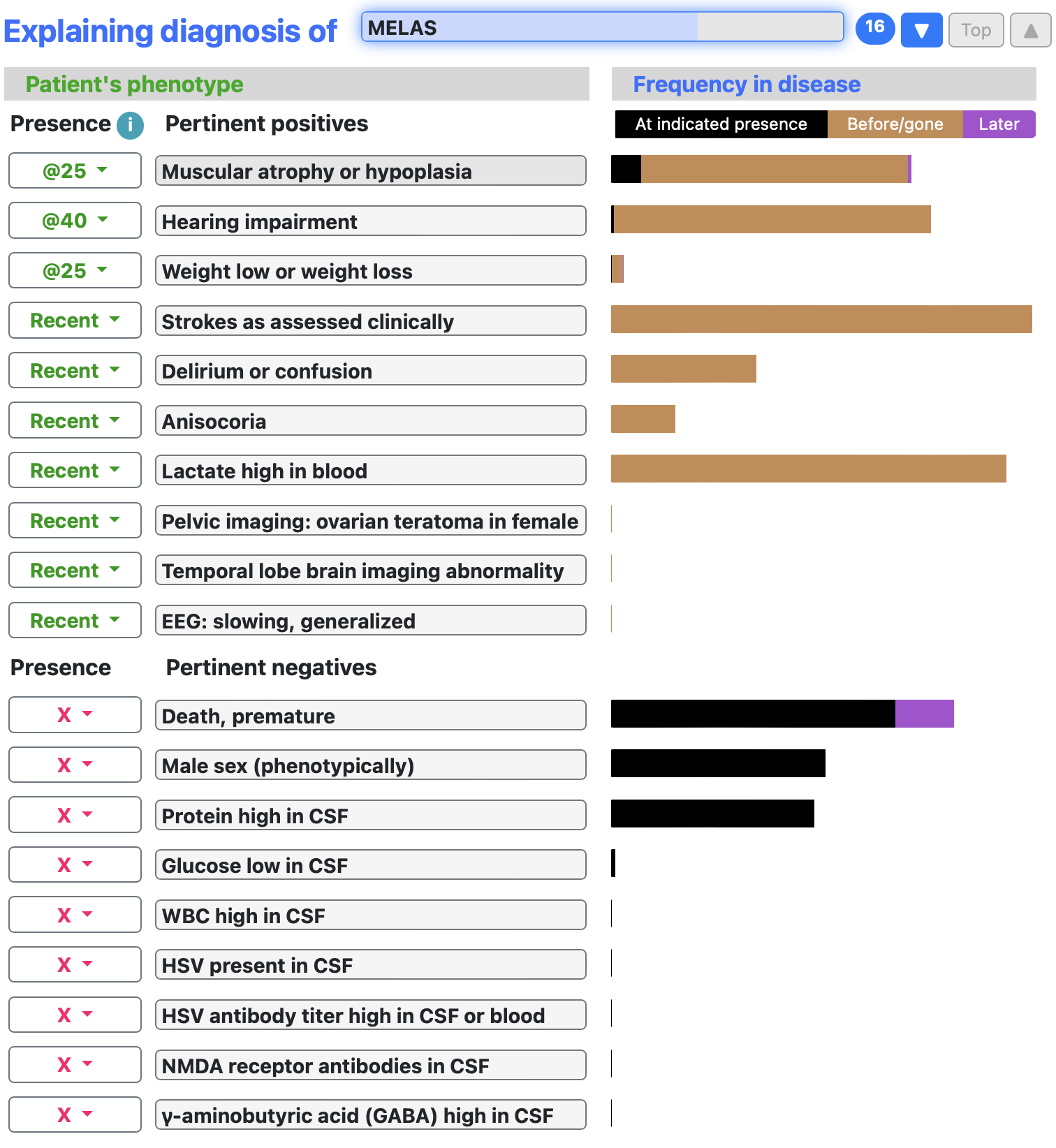
SimulConsult provides a visual explanation of the key findings that inform the differential diagnosis. This can be sorted by disease such that the viewer learns more about the selected disease and see how various findings fit within the disease state. Below we show the top three diseases identified by SimulConsult for this patient’s presentation.
MELAS (Mitochondrial Encephalomyopathy, Lactic Acidosis, and Stroke-like Episodes)
Key features in support of MELAS included stroke-like symptoms, muscular atrophy/low BMI, hearing loss and elevated serum lactate levels.
Anti-NMDA Receptor Encephalitis
Given that this patient presented with stroke like symptoms in the context of a prior teratoma, anti-NMDA Receptor encephalitis was considered. Key features that increased the likelihood of this disease were mental status changes, temporal prominence of symptoms and the presence of a teratoma.

Thiamine Deficiency
Interestingly, SimulConsult identified thiamine deficiency in the differential for this patient’s symptoms largely due to her low body weight and elevated lactate level. The presence of MRI lesions were inconsistent with this diagnosis.
Discussion of comparison between SimulConsult and Expert discussion of differential diagnosis
The expert commentary suggested that auto-immune encephalitis was a reasonable diagnosis to make at this point in the patient’s evaluation however, they note that “it is essential to rule out other possible causes of her symptoms because misdiagnosis of autoimmune encephalitis is associated with patient harm, including delays in the diagnosis and treatment of the true medical issue and complications from adverse effects of unnecessary immunosuppressive therapies.”
Mitochondrial disorder was the most likely diagnosis identified by the expert commentary due to the presence of lactic acidosis, hearing loss, low muscle mass and lack of CSF pleocytosis. SimulConsult identifies similar features and ranks MELAS first in the initial differential diagnosis.
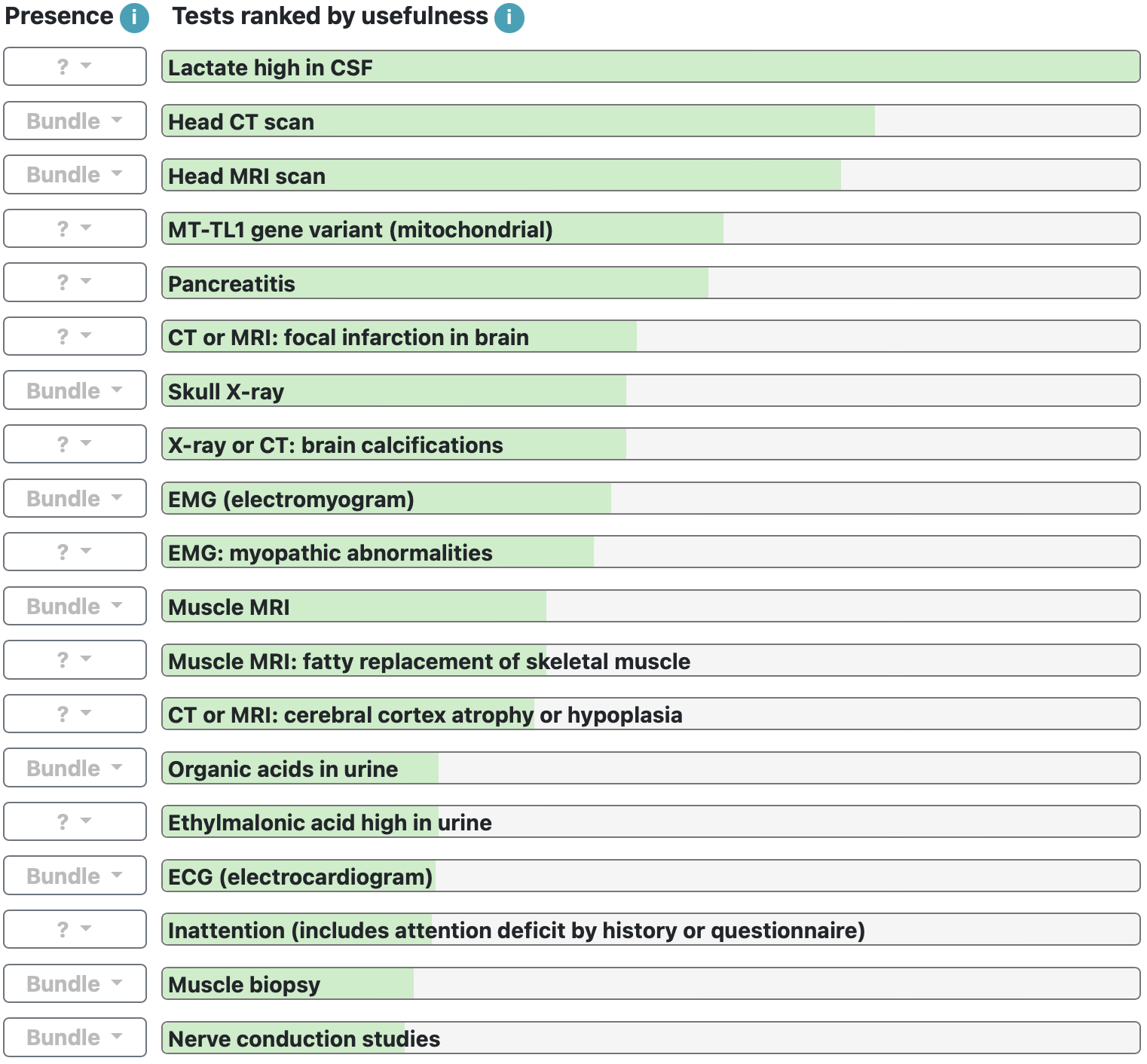
SimulConsult diagnostic testing recommendations
SimulConsult provides not only differential diagnosis but also a constantly evolving diagnostic scheme based on the relative importance of additional findings to allow for a definitive diagnosis to be made. In this case, SimulConsult suggests additional testing including:
Expert recommendations for additional Testing:
- MR spectroscopy
- Muscle biopsy
Given the ongoing diagnostic uncertainty in this case, additional diagnostic tests were performed.
A brain magnetic resonance spectroscopy study was performed which identified elevated lactate levels in the ventricular system. A muscle biopsy also identified myopathic changes consistent with a mitochondrial disorder.
- Brain Magnetic Resonance Spectroscopy
- Lactate elevated in CSF
- Muscle Biopsy:
- Mitochondrial abnormalities
- Ragged red fibers
- Myopathic changes
Identifying the Genetic Abnormality
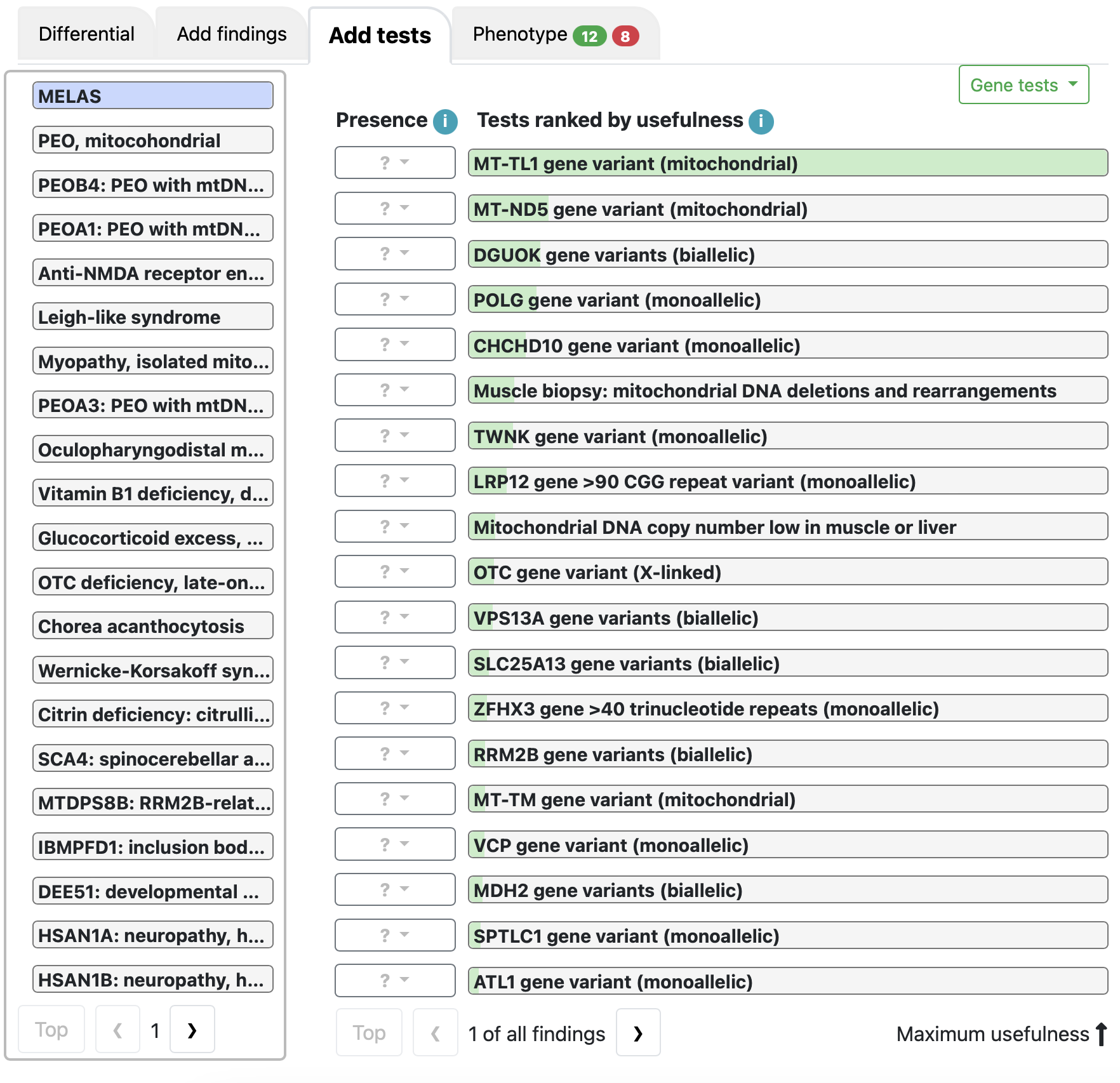
Discussion of disease based on additional testing
The presence of an elevated lactate in the CSF and mitochondrial abnormalities on muscle biopsy correctly identify the unifying diagnosis of MELAS. Subsequent genetic testing was obtained and SimulConsult correctly predicted the presence of a MT-TL1 mutation leading to MELAS syndrome.
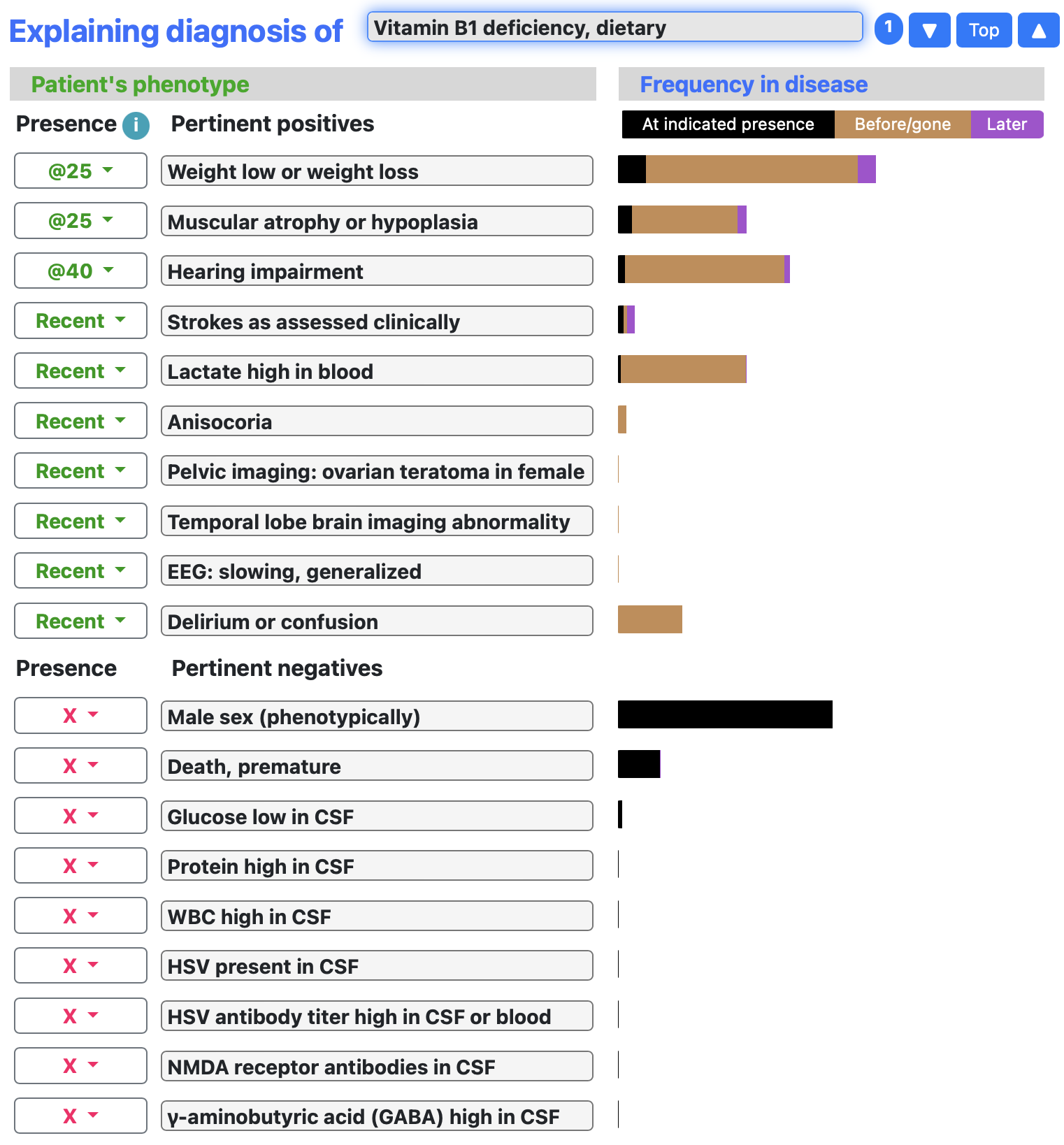
Case-Based Quality Improvement Changes
In the process of performing this case study, we identified a curious feature of the differential diagnosis. Although NMDA antibody testing was negative, NMDA encephalitis remained high on the differential diagnosis. On further investigation, we found that the frequency of anti-NMDA antibodies was present in 12 out of 12 subjects in the case series from which the anti-NMDA antibody frequency was entered into the SimulConsult algorithm. As a result of Bayesian statistics, this resulted in a ~90% sensitivity being input for this disease state. Given that further studies demonstrated that anti-NMDA antibodies are present in the CSF in essentially all cases of NMDA encephalitis we adjusted the frequency of this finding to 99% for anti-NMDA antibodies in the CSF and ~90% for anti-NMDA antibodies in the serum (Titulaer M et al. (2013) Lancet Neurol. 12:157-65). Based on the results of this clinical study, additional clinical datapoints were entered into SimulConsult system. With these changes the following differential diagnosis was identified prior to any additional diagnostic testing.
For users of SimulConsult, click the following link to load the patient profile and see for yourself how additional findings and tests can change the differential diagnosis.
There are more clinical cases here.
