The Patient Chat tool creates individualized patient questionnaires, enabling patients (or their families) to organize the pertinent parts of their history at home before the visit.
There are two types: (1) pre-diagnosis, and (2) post-diagnosis. Each version is “seeded” with some findings to help direct the questions posed to the patient. In the pre-diagnosis questionnaire, the patient’s findings from the referral are the “seed”. In post-diagnosis, the “seed” encompasses findings related to the diagnosed disease, as known at the most recent visit, and the disease itself.
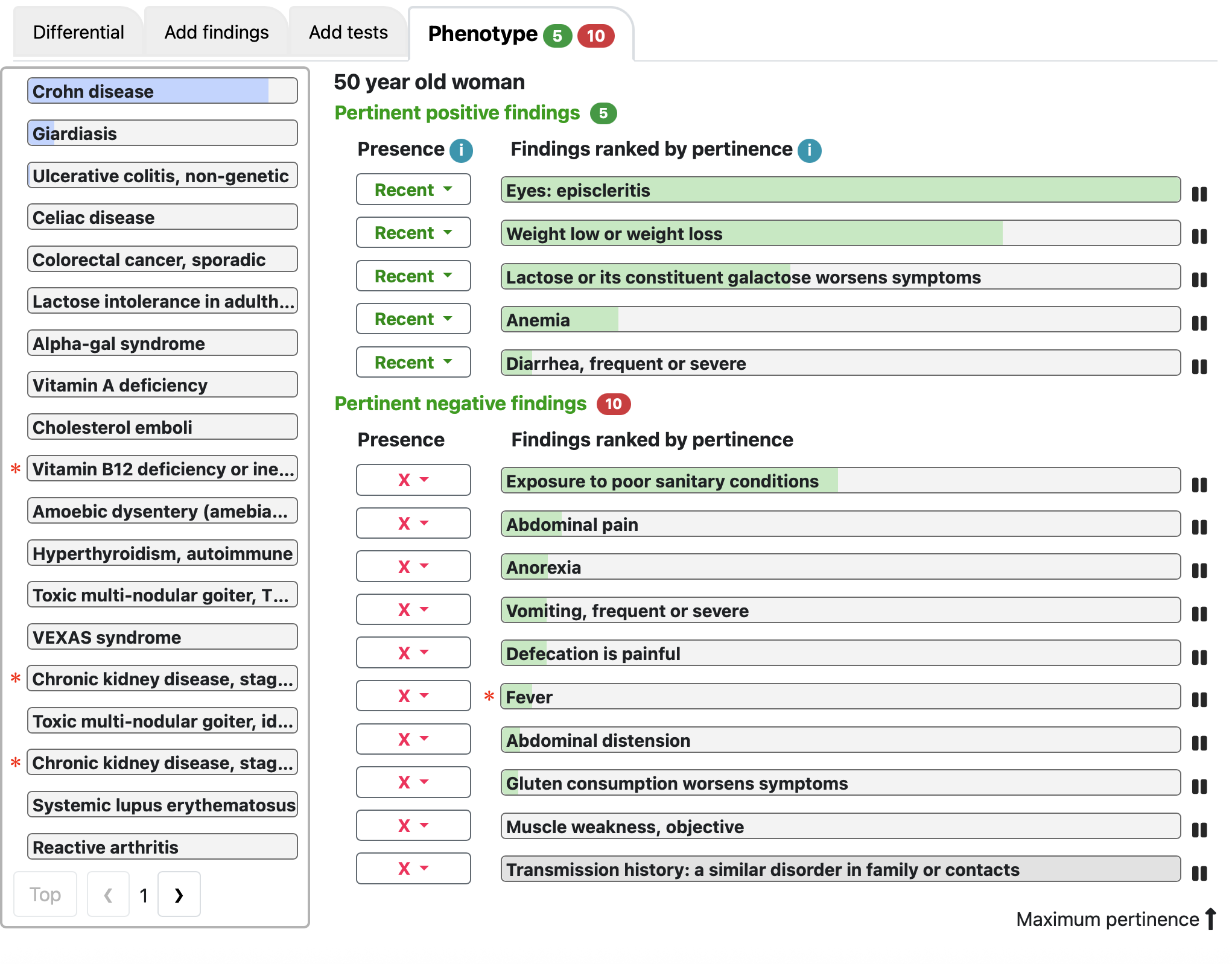
Pre-diagnosis example
The patient is a 50-year-old woman with a recent history of:
- Diarrhea
- Unexplained weight loss
- No known exposure to poor sanitary conditions.
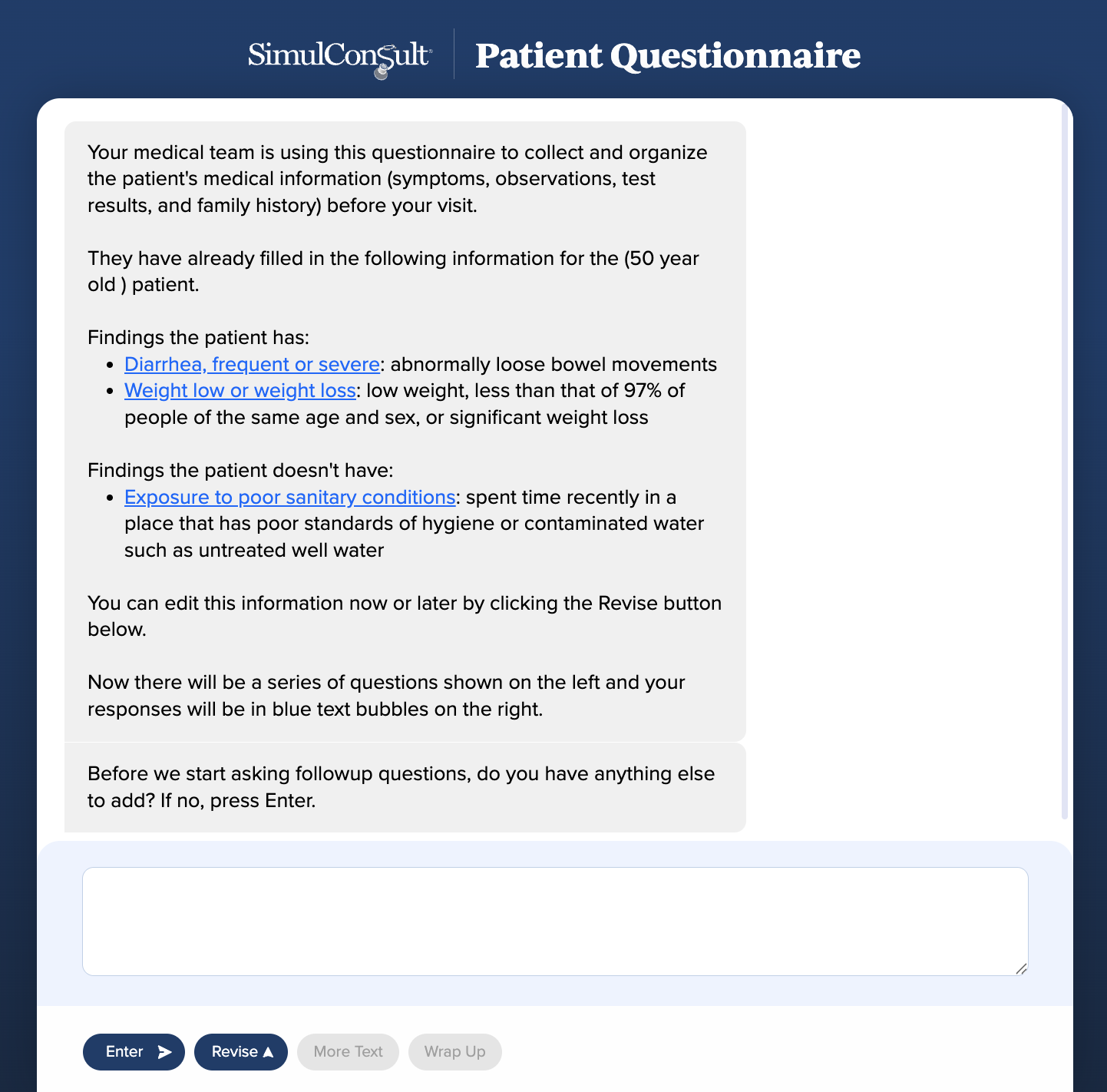
The setup is done from within the Dashboard. The staff person generates a unique survey link that can be sent to the patient via the patient portal or directly by email. In the standalone version, the staff person assigns the patient a unique survey code (not their medical record ID) and then tracks the replies and forwards them to the clinician on an identified basis, within the institution’s email system.
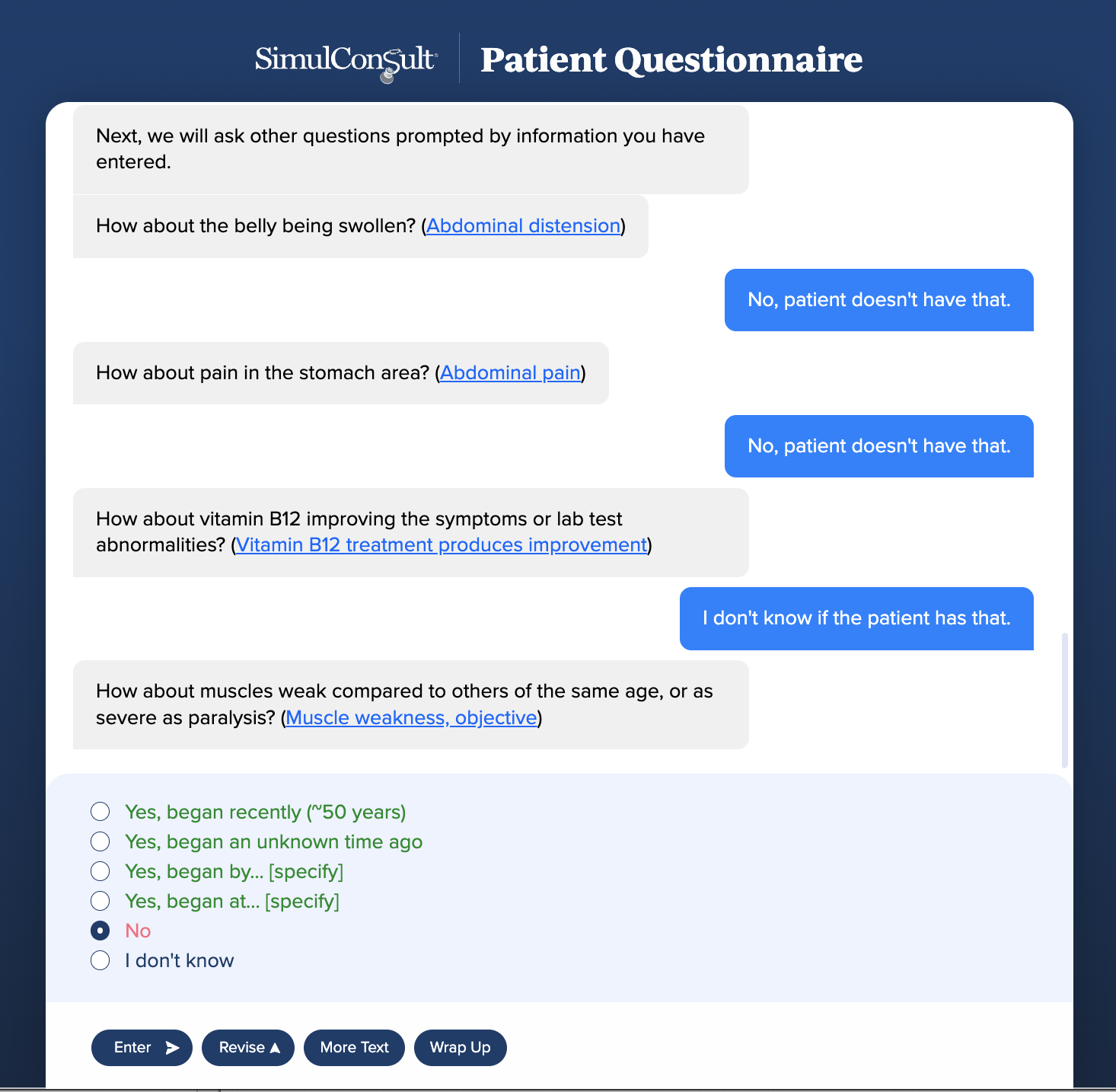
Next, new information is gathered one question at a time, including a brief set of questions relating to family history and exposure.
The logic of the Patient questionnaire relies on the same powerful diagnostic engine as the clinician tools.
- In the pre-diagnosis questionnaire, each question is driven by the usefulness of the information to narrow the differential diagnosis. (Note: the differential diagnosis is NOT shared with the patient.)
- In the post-diagnosis questionnaire, the questions are in the order of the frequency of those findings in the diagnosed disease, at the patient’s age.
The results are returned to the staff person who set up the questionnaire, who can then share them with the clinician seeing the patient, in the Dashboard Phenotype. The questionnaire avoids certain relevant findings that patients are unlikely to be able to assess. It also has lay explanations of each finding, where non-obvious, and links to more information.
The process relies on the clinician to review the findings and refine the history and exam as needed, in the process of arriving at a diagnosis or developing a testing plan to reach one. The objective is to save the clinician time, and ensure the patient feels they had a chance to fully present their history.
Patients will often include findings that the clinician believes are related to another condition the patient might have or is known to have. The Pause/Play allows the clinician to quickly move seemingly irrelevant findings to the background while retaining the full list reported by the patient.